Claudia Zimmerman, a registered nurse with nearly 25 years of experience, faced significant challenges after undergoing medically induced early menopause at the age of 29. This experience profoundly impacted her personal life and career as a nurse manager, leading to nearly two decades of struggles with anxiety, hot flashes, and weight gain. It wasn’t until she gained access to menopause-specific healthcare and support at work that her well-being began to improve.
Zimmerman’s journey into early menopause began with a diagnosis of stage three endometriosis, a painful condition where tissue grows outside the uterus. Despite her expertise in women’s reproductive health, she found herself dismissed by multiple physicians who downplayed her symptoms. Frustration mounted as she struggled with excruciating pain, ultimately prompting her to make the difficult decision to undergo a hysterectomy.
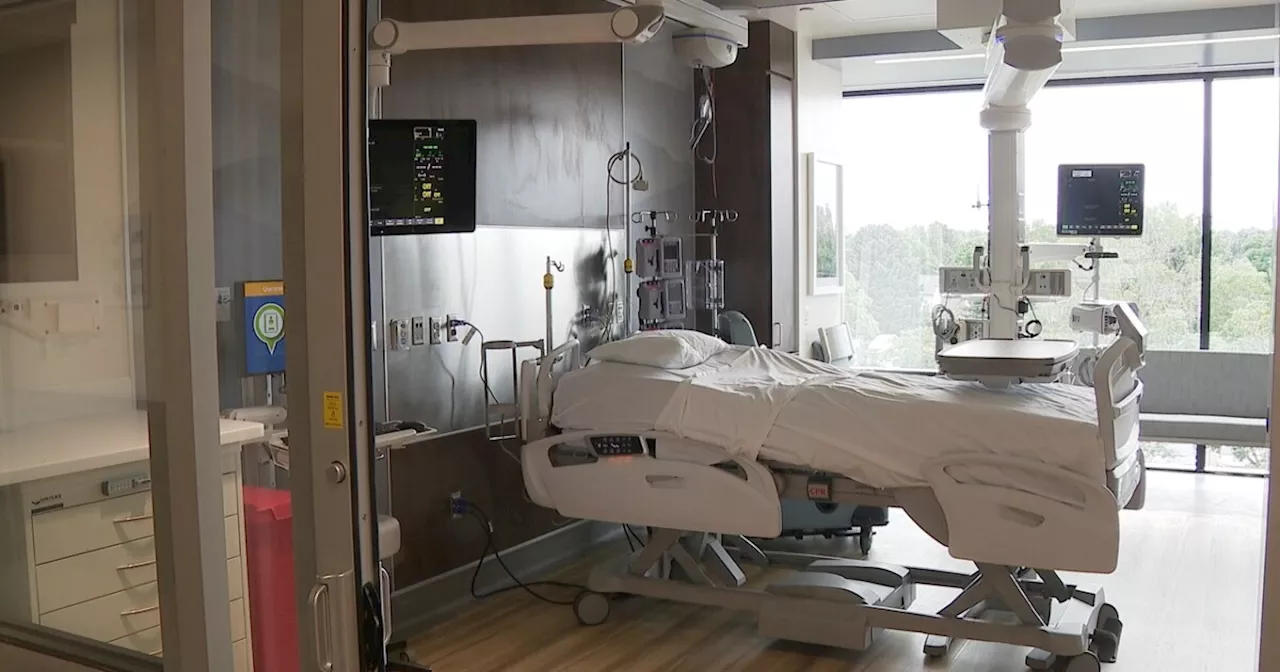
The surgery removed her ovaries, cervix, and uterus, placing her into medically induced early menopause. Although she was somewhat aware of menopause symptoms, nothing could have prepared her for the intensity of the experience. Initially, she managed to delay the onset of menopause due to an ovarian remnant producing estrogen. However, after its removal two years post-hysterectomy, she faced the full brunt of menopausal symptoms.
Working full-time as an IVF nurse during this period posed its own unique challenges. The onset of anxiety, weight gain, and depression coincided with the arrival of hot flashes. Zimmerman described these hot flashes as a sudden panic that would engulf her, often leaving her drenched in sweat regardless of her surroundings.
Being open with her colleagues about her experiences proved beneficial. Many of her coworkers, also women, provided support and shared advice on managing symptoms. Zimmerman employed various strategies to cope, such as consuming iced water and taking breaks to walk and talk with her mother, who had always been a source of emotional support.
Despite her efforts, Zimmerman grappled with feelings of self-consciousness related to weight gain, often opting for larger scrubs to conceal her changing body. Her role as a patient-centric nurse required frequent interactions, which added to her anxiety on days when she felt less than her best.
The emotional toll of her condition continued to escalate, leading to resentment and short temper, especially as she juggled the demands of being a mother and wife. The pressure of her responsibilities made it difficult to find restful sleep, further exacerbating her symptoms.
After ten years at the fertility clinic, Zimmerman transitioned to a new role in benefits management with Progyny, a company focused on fertility and women’s health. Shortly after this change, her menopause symptoms peaked, coinciding with the loss of her mother to ovarian cancer.
The demands of her new job, which allowed her to work from home, provided a semblance of relief. No longer needing to mask her symptoms in front of patients or colleagues, she focused on her work, but the impact on her family became increasingly evident.
While developing menopause-specific benefits at Progyny, Zimmerman discovered the availability of menopause-certified clinicians through a digital health platform. This revelation prompted her to schedule an appointment with a specialist, marking a pivotal moment in her journey.
The appointment proved transformative. The nurse practitioner attentively listened to Zimmerman’s struggles and developed a tailored care plan that included three new medications. As a result, she regained the ability to sleep through the night and lost 25 pounds, all while achieving balanced hormones.
Zimmerman’s experience highlights the critical need for employers to acknowledge the unique healthcare challenges faced by women, particularly in relation to menopause. She emphasizes that providing access to specialized care and offering an empathetic ear can significantly improve the lives of women in the workplace.
Reflecting on her journey, Zimmerman wishes she had known earlier to advocate for her own health. Now, she encourages others to seek the support they need, reassuring them that conditions can improve with the right help.